- Pioneer of Hair Transplant with world's latest & Best Technique FUT, in up
- Excellent Quality Hair Transplantation by highly Skilled & Experienced Plastic Surgeon
- Pioneer of Hair Transplant with scar less technique FUE, in up
- World class surgery at affordable cost with life changing results
- Pioneer of body hair to scalp transplant in up
- Many thousand patients with successful Hair Transplant results
Quick Contact
revivecliniclko@gmail.com
+91 9721476547, +91 8400746979

Other Plastic Surgery Procedures
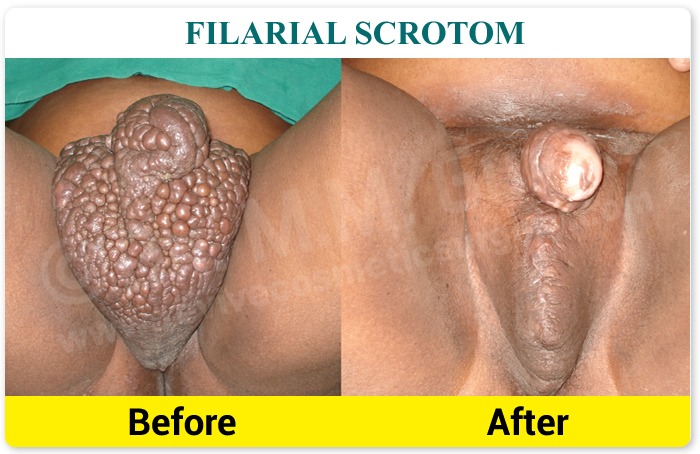
Plastic & Reconstructive surgeries are performed to treat structures of the body affected aesthetically or functionally by congenital defects, developmental abnormalities, trauma, infection, tumors or disease. It is generally done to improve function and ability, but may also be performed to achieve a more typical appearance of the affected structure.
Breast Reconstruction
The goal of breast reconstruction is to restore one or both breasts to near normal shape, appearance, symmetry and size following mastectomy, lumpectomy or congenital deformities.
Breast reconstruction often involves multiple procedures performed in stages and can either begin at the time of mastectomy or be delayed until a later date.
Breast reconstruction generally falls into two categories: implant-based reconstruction or flap reconstruction. Implant reconstruction relies on breast implants to help form a new breast mound. Flap (or autologous) reconstruction uses the patient's own tissue from another part of the body to form a new breast.
Cleft Lip and Cleft Palate repair Surgery
The incomplete formation of the upper lip (cleft lip) or roof of the mouth (cleft palate) can occur individually, or both defects may occur together. The conditions can vary in severity and may involve one or both sides of the face.
Cleft lip and cleft palate repair is a type of plastic surgery to correct this abnormal development both to restore function and to restore a more normal appearance.
Most clefts can be repaired through specialized plastic surgery techniques, improving your child's ability to eat, speak, hear and breathe, and to restore a more normal appearance and function.
Hand Surgery
If your hand is impaired in any way, surgery may improve your condition. This type of very specialized surgery can treat diseases that cause pain and impair the strength, function and flexibility of your wrist and fingers. Surgery seeks to restore to near normal the function of fingers and hands injured by trauma or to correct abnormalities that were present at birth. Hand surgery can treat-
- Carpal tunnel syndrome: A condition caused by pressure to the median nerve within the wrist, or carpal tunnel. You might feel pain, a tingling sensation, numbness of the fingers, weakness or aching. Carpal tunnel syndrome is associated with multiple conditions including: repetitive motion or overuse, fluid retention during pregnancy, injury to the nerve in the carpal tunnel or rheumatoid arthritis.
- Ganglion removal- They can occur on the fingers, hands or wrists. They start as very small lumps and grow in size in varying degrees. If left untreated the lump can grow in size and can eventually cause discomfort and loss of movement where it will require removal through surgery. Downtime is minimal but might require physiotherapy.
- Trigger Fingers- Trigger finger/thumb occurs when the pulley at the base of the finger becomes too thick and constricting around the tendon, making it hard for the tendon to move freely through the pulley. Sometimes the tendon develops a nodule (knot) or swelling of its lining. Because of the increased resistance to the gliding of the tendon through the pulley, one may feel pain, popping, or a catching feeling in the finger or thumb.
Causes for this condition are not always clear. Some trigger fingers are associated with medical conditions such as rheumatoid arthritis, gout, and diabetes. Local trauma to the palm/base of the finger may be a factor on occasion, but in most cases there is not a clear cause.
This surgery is performed as an outpatient, usually with simple local anesthesia. The goal of surgery is to open the pulley at the base of the finger so that the tendon can glide more freely. Active motion of the finger generally begins immediately after surgery. - Tendon & Neuro-vascular Injuries- Both flexor or extensor tendons may be injured because of many type of trauma. Neuro-vascular injuries are also associated with many of these injuries. These can be repaired with sophisticated plastic & Micro surgical technique to restore fingers/ hands movement, sensation and their vascularity.
- Fractured Fingers and Hands- Dr Gupta also treat patients with emergency conditions such as fractures to the hands and fingers. These conditions should be treated at earliest after sustaining the injury to ensure full rehabilitation.
- Micro-vascular Re-implantation of Hand/ Digits- If hand or part of it is amputated because of some sharp cut, they can be re-implanted by microsurgical technique provided part is brought in proper condition and surgery is done within 5-6 hours.
- Tendon Transfer- In cases of isolated or combined nerve palsy, following trauma or some disease, hands are deformed and pts are not able to perform many basic functions. These deformities can be corrected and functions can be restored by doing tendon transfer of functioning muscles to replace actions of non functioning muscles.
- Congenital Hand Abnormalities-
a. Synductyly- a condition wherein two or more digits are fused together.
b. Polyductyly- a condition of having supernumerary/ extra fingers or toes.
Maxillofacial Injuries including Facial bone/ Jaw Fractures
Facial trauma, also called maxillofacial trauma, is any physical trauma to the face. Facial trauma can involve soft tissue injuries such as burns, lacerations and bruises, or fractures of the facial bones such as Mandibular fractures, Maxillary (Le Fort) fractures, Zygomatic/ zygomatico-maxillary complex fractures, Nasal fractures, Orbital fractures. Symptoms are specific to the type of injury; for example, fractures may involve pain, swelling, loss of function, or changes in the shape of facial structures.
Injury mechanisms such as falls, assaults, sports injuries, and vehicle crashes are common causes of facial trauma.
CT scanning is usually considered to be more definitive and better at detecting facial injuries than X-ray.
Treatment aims to repair the face's natural bony architecture and to leave as little apparent trace of the injury as possible. Fractures may be repaired with Titanium mini plates and screws. They may also be wired into place. Bone grafting is another option to repair the bone's architecture, to fill out missing sections, and to provide structural support. Medical literature suggests that early repair of facial injuries, within hours or days, results in better outcomes for function and appearance.
Dr. Gupta is highly trained and experienced in the comprehensive management of trauma to the lower, middle and upper face and assure better out come in term of minimum scarring & best functional result.
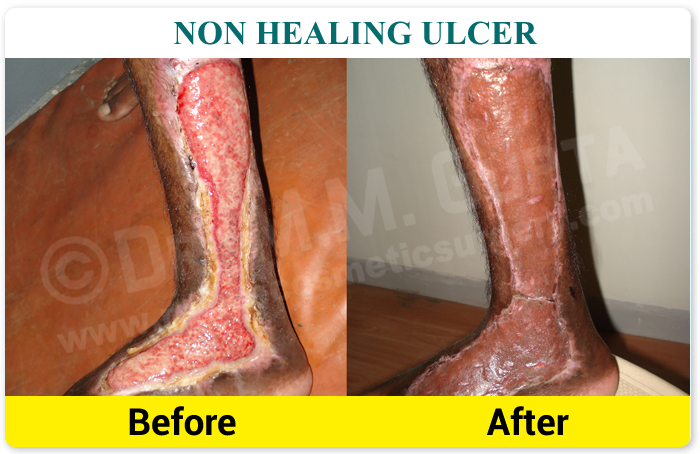
Non Healing Ulcers/ Chronic Wound
A chronic wound is a wound that does not heal in an orderly set of stages and in a predictable amount of time the way most wounds do; wounds that do not heal within three months are often considered chronic.
These wounds cause patients severe emotional and physical stress and create a significant financial burden on patients and the whole healthcare system.
In addition to poor circulation, neuropathy, and difficulty moving, factors that contribute to chronic wounds include systemic illnesses, age, and repeated trauma.
The vast majority of chronic wounds can be classified into three categories: venous ulcers, diabetic ulcers, and pressure ulcers.
Optimal management of wounds requires holistic assessment. Though treatment of the different chronic wound types varies slightly, appropriate treatment seeks to address the problems at the root of chronic wounds, including ischemia, bacterial load, and imbalance of proteases. Peri-wound skin issues should be assessed and their abatement included in a proposed treatment plan. Various methods exist to ameliorate these problems, including antibiotic and antibacterial use, debridement, irrigation, vacuum-assisted closure, warming, oxygenation, moist wound healing, removing mechanical stress, and adding cells or other materials to secrete or enhance levels of healing factors.
The challenge of any treatment is to address as many adverse factors as possible simultaneously, so each of them receives equal attention and does not continue to impede healing as the treatment progresses.
Burn & Post Burn Deformities
Acute Burn
A burn is a type of injury to skin, or other tissues, caused by heat, cold, electricity, chemicals, friction, or radiation. Most burns are due to heat from hot liquids, solids, or fire.
Treatment depends on the severity of the burn. Superficial burns may be managed with little more than simple pain medication, while major burns may require prolonged treatment in specialized burn centers. Partial-thickness burns may require cleaning with soap and water, followed by dressings. Full-thickness burns usually require surgical treatments, such as skin grafting. Extensive burns often require large amounts of intravenous fluid, due to capillary fluid leakage and tissue swelling. The long-term outcome is related to the size of burn and the age of the person affected.
Post Burn Deformities
Third degree burns may cause serious deformity or hideous disfigurement. By definition, third degree burns are those which destroy the entire thickness of the skin and more or less underlying tissue. Such wounds heal slowly by granulation, cicatrization, and ingrowths of epithelium from the edges. In general the deformities depend chiefly upon the location and the extent of tissue destruction. A contracture may cause limitation of movement if present on a joint or it may lead to unsightly appearance of the affected part due to pull on the surrounding healthy tissues. The end-result of such a healing process may be greatly improved by proper surgical treatment.
Post burn deformities include- Contractures, Scarring (Hypertrophic or Keloid), Hypopigmentation or Hyperpigmentation of healed area. The broad diffuse contractures generally respond well to release and insertion of a skin graft or substitute, whereas the linear band-like contractures are generally repaired using a simple or modified Z-plasty or a transpositional flap technique. Treatment of burn deformities is provided through multiple surgeries spaced across a period of many years.
Tissue expander promotes the growth of extra skin by stretching the surrounding tissue and this newly grown skin is used to replace the damaged skin.
The pulsed dye laser is a promising technique used to reduce scar thickness and redness.
Steroid injections, silicone gel sheet and Pressure garments reduce thick scars and treat itchiness.
Photo Gallery FAQWhat makes us unique?
Our Efficiency | Our Competency | Our Reliability | Our Dedication | Our Expertise in the respective fields.
Best Doctors
We have a team of doctors who are best in their respective fields of specialization for best results and maximum patient safety.
Best Plastic & Cosmetic Surgeon
MBBS, MS, MCh, DNB
- Our plastic and cosmetic surgeon are highly trained and best Hair Transplant Surgeon with more than 14 years of experience in doing Hair Transplant with excellent & world-class results.
- The most trusted, skilled, and experienced Hair Transplant and Cosmetic Surgeons in Lucknow and Varansi is owned by Revive Clinic
- Our surgeon is a Pioneer of the FUT technique of Hair Transplant in Uttar Pradesh.
- Our surgeon is a Pioneer of the FUE technique of Hair Transplant in Uttar Pradesh.
Best Gynecological Surgeon
MBBS, DGO, DNB
- Our gynecological and obstetrics doctor is highly trained Obstetrician, Gynecologist & Laparoscopic Surgeon with more than 17 years of experience.
- Our gynecological and obstetrics doctor is working as a Senior Consultant Obstetrician & Gynecologist at Fatima Hospital, Lucknow.
- Revive Clinic posseses one of the best and highly experienced Obstetrics & Gynecology & Laparoscopic doctors in Lucknow.
Ultra-modern Centre
Hair Transplant Center
- We have state of art ultra-modern facility for hair transplant. We use ultra-hygienic and the best safety method for patient care.
- We have a dedicated Hair Transplant Operation Theater (Hair Lab.) with temperature and humidity control, ergonomically designed cutting platform, cold lights, ceiling lights with heat filters, preventing any damage to the Hair grafts.
- Revive Clinic is one of the leading hair transplant clinics in Lucknow, Uttar Pradesh, India. Our hair treatment procedures are best in class and give the best results.
- We offer the best hair transplant treatment with all the latest and best techniques & instruments.
- We ensure maximum patient's privacy, it is our first priority.
Obstetrical & Gynecology Treatment
- We have advanced facilities & equipment for providing the best obstetrical & gynecological treatment.
- All treatments are done by our highly experienced doctor taking utmost care for giving the best results and high priority for patient safety.
- At Revive we evaluate every patient for normal delivery as a primary option, doctor opt for caesarian delivery only in high-risk conditions for the safety of mother and baby.
- Revive clinic is one of the best obstetrical & gynecological clinics in Lucknow.
- Revive Clinic offers a wide range of obstetrical & gynecological care i.e. From contraceptive counseling to general gynecological & obstetrical services including Infertility Treatment for women at different stages of life, we are best in our field.
Best Results
- Our success is well spoken by thousands of our happy and satisfied patients of Hair Transplant & Plastic & Cosmetic Procedures both national as well as international. We are committed to patient's safety & satisfaction.
- 100% natural-looking results are given by our best hair transplant and cosmetic surgeon, with no side effects.
- We provide the best hair transplant & cosmetic Surgery results at very affordable costs.
- We have excellent results for infertility treatment.
- We give the best results for all Obstetric & Gynecological problems at a very affordable cost.
Professional Staff
Why us

State of Art CenterLatest Equipment & Techniques

- We use latest Equipments & Techniques to deliver top class Treatments
- Our center have relaxing environment with modern facilities and look
Qualified Doctor & StaffBoard Certified and Specialized Team

- Dr. M. M. Gupta is; experienced, highly qualified and skilled cosmetic surgeon; providing surgical services of International Standard.
- Our team consists of trained and caring staffs, available 24x7 for patient's care.
World Class ResultsMaximum Patient Satisfaction

- Combination of State of Art Center and Experienced, Highly Qualified & Skilled Cosmetic Surgeon bring out world class results, every patient expect.
- You can see Live Surgical Procedures and also meet our satisfied clients to gain confidence about our Excellent Results.

Our Specialities



Quick Contact
revivecliniclko@gmail.com
+91 9721476547, +91 8400746979
Mail Your Query Here

Credentials
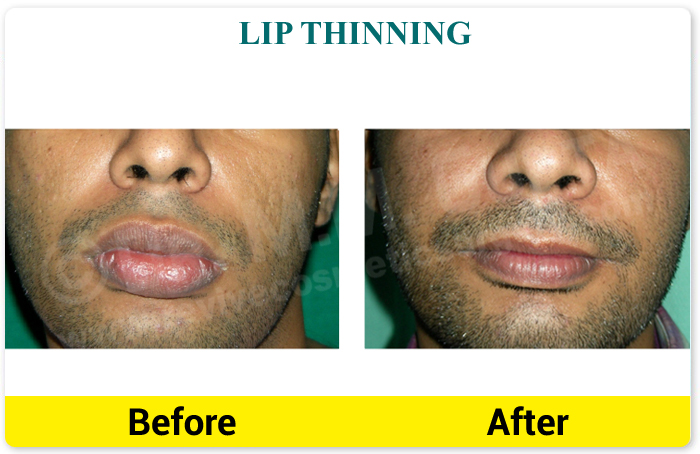
Face
Hair & Skin
Body
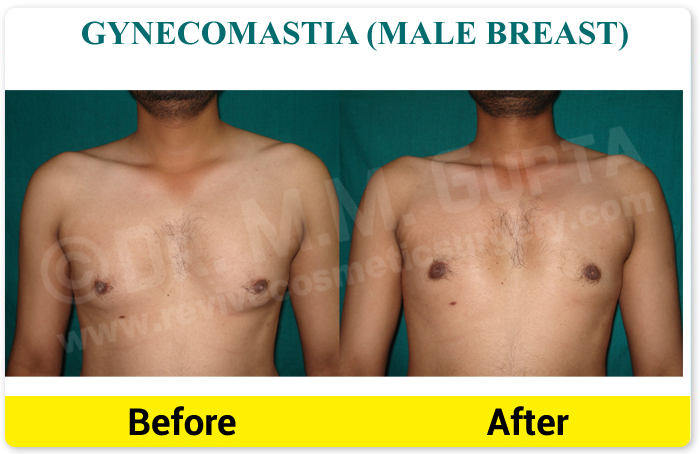
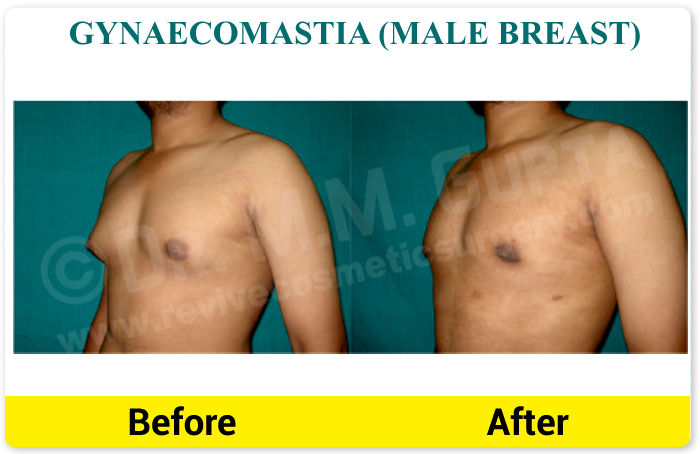
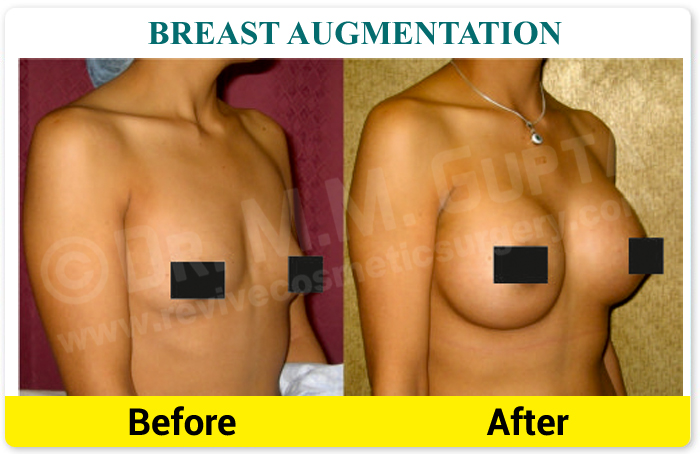
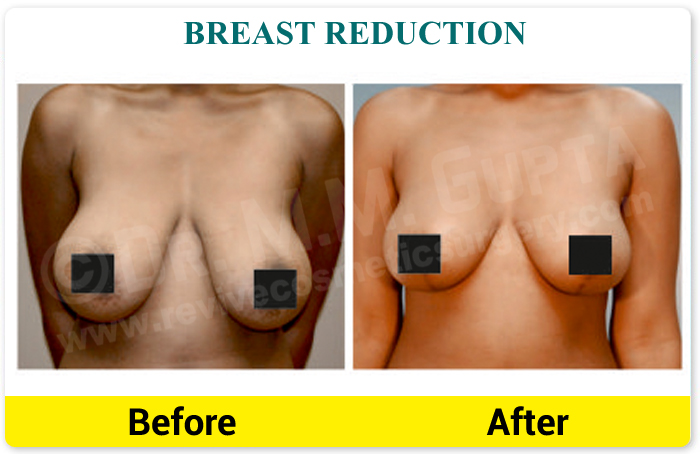
Breast